Distinguishing Between Walking and Running Shoes

Differentiating between walking and running shoes is essential for optimizing comfort and performance during physical activity. While both types of shoes may appear similar, subtle design features cater to the distinct biomechanics and movement patterns associated with each activity. Running shoes typically feature more cushioning and support in the heel and forefoot to absorb impact and provide stability during high-impact movements. They also tend to have a more flexible sole to facilitate the rolling motion of the foot from heel to toe. In contrast, walking shoes prioritize flexibility in the forefoot and emphasize support and stability throughout the midsole to accommodate the heel-to-toe motion of walking. Additionally, walking shoes often have a lower profile and lighter weight compared to running shoes. Understanding these differences allows individuals to select the appropriate footwear for their preferred activity, ensuring optimal comfort, support, and injury prevention during walking or running endeavors. If you have more specific questions about what type of shoes to buy for your walking or running experiences, it is suggested that you consult a podiatrist.
For more information about walking shoes versus running shoes, consult with one of our podiatrists from Podiatry Services . Our doctors can measure your feet to determine what your needs are and help you find an appropriate pair of footwear.
Foot Health: The Differences between Walking & Running Shoes
There are great ways to stay in shape: running and walking are two great exercises to a healthy lifestyle. It is important to know that running shoes and walking shoes are not interchangeable. There is a key difference on how the feet hit the ground when someone is running or walking. This is why one should be aware that a shoe is designed differently for each activity.
You may be asking yourself what the real differences are between walking and running shoes and the answers may shock you.
Differences
Walking doesn’t involve as much stress or impact on the feet as running does. However, this doesn’t mean that you should be any less prepared. When you’re walking, you land on your heels and have your foot roll forward. This rolling motion requires additional support to the feet.
Flexibility – Walking shoes are designed to have soft, flexible soles. This allows the walker to push off easily with each step.
If you have any questions, please feel free to contact our office located in Murrieta, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Differences between Walking and Running Shoes
Both running and walking are great exercises, but should a person wear the same shoes for both activities? The answer is no, because there is a difference between the way a person’s feet hit the ground when they are walking and when they are running. Therefore, the shoes for each activity are designed differently. Before you begin any exercise program it is always recommended that you speak with your doctor or podiatrist.
Walking is a low impact exercise that is often recommended by doctors to their patients. While walking is a simple activity, it still requires some degree of preparation. If you think about walking and how your feet strike the ground as you move, you will notice that your heel hits the ground first before your foot continues to roll forward and your next step begins. Because of this rolling motion, walking shoes are designed to be more flexible than running shoes. This flexibility helps the walker push off with each step taken.
Because the heel hits the ground first when you walk, walking shoes are designed to absorb most of the shock. Walking shoes should therefore have a beveled or angled heel. The angle of the heel helps absorb the shock and reduces pressure from the ankles. This is especially important for speed walkers, as their feet will hit the ground twice as often as the normal walker.
When people decide to run as a hobby or for their health, they must first realize that running is a high impact exercise. If not done with the proper equipment, running may cause damage to the feet and legs. Running shoes are designed to be more lightweight and to have thicker soles. The thicker soles act as shock absorbers for the rest of the body. Walking shoes often do not have the proper arch support that running shoes do.
A proper fitting shoe can make or break a runner or a walker. If the shoes are too big, their feet will slide back and forth inside the shoe and cause blisters. Whether you will be running or walking, the right equipment can make all of the difference in the world.
Morton’s Neuroma Explained
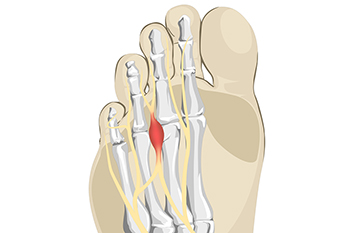
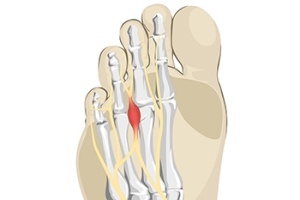
Foot pain, particularly sharp and stabbing sensations that ease when you stop walking and massage your foot, may indicate Morton's neuroma. Despite its intimidating name, this condition is typically harmless and very treatable. A neuroma, in simple terms, refers to the thickening of a nerve between the toes, usually between the second and third toes. Rarely, it can affect the space between the fourth or first toe. Morton's neuroma may also be called intermetatarsal neuroma, interdigital neuroma, Morton's metatarsalgia, perineural fibrosis, or entrapment neuropathy. Common symptoms can include sharp pain, numbness, tingling, burning, cramping, and a sensation of stepping on an object. Relief is often found by removing the shoe and massaging the foot. The exact cause of this nerve injury is unclear, but it may result from various factors, including foot structure, biomechanical abnormalities, and wearing ill-fitting shoes. Women aged 30 to 50 are more susceptible. Diagnosis involves a physical exam, including compression tests, and sometimes imaging such as X-rays, ultrasounds, or MRIs. To prevent Morton's neuroma, opt for well-fitting, comfortable shoes with wide-toe boxes, avoid high heels and narrow shoes, and consider orthotic inserts if needed. If you have pain in the area described above, it is suggested that you schedule an appointment with a podiatrist for a proper diagnosis and care.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact one of our podiatrists of Podiatry Services . Our doctors will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our office located in Murrieta, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Morton's Neuroma
Morton's Neuroma, also called Intermetatarsal Neuroma or Plantar Neuroma, is a condition that affects the nerves of the feet, usually the area between the third and fourth toe. Neuroma refers to a benign growth that can occur in different parts of the body. Morton's Neuroma strictly affects the feet. This condition causes the tissue around the nerves that lead to the toes becoming thick, causing pain in the ball of the foot.
This condition can be caused by injury, pressure or irritation. Normally no lump will be felt, but instead burning pain in the ball of the foot will be experienced. Numbness and tingling may also occur. With the onset of this condition, a person may feel pain when tight or narrow shoes are worn. As the condition worsens, the pain may persist for days, or even weeks.
Persistent foot pain should always be a concern. The foot should be examined by a podiatrist if pain persists longer than a few days with no relief from changing shoes. The earlier the foot is examined and treated, the less chance there will be for surgical treatment.
There are some factors that can play a role in the development of Morton's Neuroma. These include wearing ill-fitting shoes that cause pressure to the toes, such as high heels. Also, high impact exercise may contribute to the cause of this condition. Morton’s Neuroma may also develop if the foot sustains an injury. Another cause includes walking abnormally due to bunions or flat feet. This causes excessive pressure and irritates the tissue. At times, people are affected for no determinable reason.
Podiatrists can alleviate the effects of this condition using a treatment plan to help decrease the pain and heal the foot tissue. Depending upon the severity of the Morton's Neuroma, the treatment plan can vary. For cases that are mild to moderate, treatments may include applying padding to the arch to relieve pressure from the nerve and reduce compression while walking. Ice packs can also help reduce swelling. The podiatrist may also create a custom orthotic device to support the foot and reduce compression and pressure on the affected nerve. The doctor will probably advise against partaking in activities that cause constant pressure on the affected area. They may provide wider shoes to ease the pressure from the toes. If these treatments do not relieve the symptoms of this condition, the doctor may use injection therapy.
Surgical treatment may be recommended by the podiatrist if all other treatments fail to provide relief. Normally, the podiatric surgeon will decide on either a surgical procedure that involves removal of the affected nerve or will choose surgery to release the nerve. After examination, the surgeon will decide on the best approach to treat the problem.
Recovery varies according to the type of surgical procedure. The patient will also be instructed on the best shoe wear to prevent the return of this condition, along with changes to workout routines, if this was a cause. Preventative measures are important in ensuring the condition does not return.
Pros and Cons of Laser Treatment for Toenail Fungus

Laser treatment for toenail fungus has emerged as a popular option for those seeking an alternative to traditional remedies. One of the notable advantages lies in its non-invasiveness, as the procedure is typically painless and requires no anesthesia. Laser therapy targets the fungal infection by penetrating the nail, effectively destroying the fungi without harming surrounding tissues. The absence of side effects and a relatively short treatment duration are additional pros that attract individuals to this method. However, it is essential to consider the drawbacks. Laser treatment may require multiple sessions for optimal results, making it a potentially lengthy process. Moreover, the effectiveness can vary, and its success is contingent on the severity of the fungal infection. Weighing these pros and cons is essential for individuals contemplating laser treatment for toenail fungus to make informed decisions about their foot health. If you have developed toenail fungus, it is suggested that you discuss treatment options with a podiatrist who can determine if laser treatments are the right option for you.
Laser treatment can be an effective way to get rid of toenail fungus. If you have any questions about laser treatment, consult with one of our podiatrists from Podiatry Services . Our doctors will assess your condition and provide you with quality treatment for fungal nails.
What Are Toenail Fungal Infections?
Onychomycosis, or fungal infection of the nail, is a relatively common and non-serious condition. Around 10 percent of U.S. citizens are afflicted with fungal nails. Common forms of fungus that infect the nail include dermatophytes, yeasts, and molds.
Symptoms of Toenail Fungal Infections Include:
- Nail thickening
- Brittleness of the nail
- Discoloration of the nail
Diagnosis for Fungal Nails
Fungal infections are diagnosed by fungal culture and microscopy. This will rule out any other conditions such as nail trauma, psoriasis, lichen planus, and onychogryphosis.
What Is Laser Treatment?
Laser treatment is a non-invasive, safe, quick, and painless procedure that uses the heat from a laser to kill fungus in the nail. Each infected nail is targeted with a laser for several minutes. The treatment is usually utilized several different times over a select period. During this time, a podiatrist will keep an eye on the infection.
If you have any questions, please feel free to contact our office located in Murrieta, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Laser Treatment for Fungal Nails
A new treatment for fungal nails, or onychomycosis, which has grown in popularity in recent years, is laser treatment. Laser treatment involves the use of a laser that kills fungus in the toenail with heat. Laser therapy causes no side effects and does not affect nearby healthy tissue.
Toenail fungus afflicts almost 10 percent of the U.S. population and is more common among the elderly. The most common symptom of toenail fungus is the discoloration and thickening of the nail. The nail can also become brittle and a foul smell may be produced. In rare cases, pain might be present. While it is not a serious condition, it can lead to a perception of disgust amongst those it affects. There are several different fungi that cause fungal infections. These include dermatophyte, yeast, and mold. The most common of these is dermatophyte.
Diagnosis for fungal nails involves a podiatrist utilizing microscopy and fungal cultures. This will allow the doctor to determine whether it is a fungus or another condition, such as lichen planus, psoriasis, nail damage, and onychogryphosis.
Fungus in the nails can be hard to get rid of with over-the-counter drugs. This is due to the nail being hard and protective, with fungus able to slip between the nail bed and plate. Furthermore the slow growth of the nail increases the difficulty of fungus going away. Laser treatment seeks to get around this by directly penetrating through the nail and killing the fungus. The laser is used on each infected nail for a couple of minutes. Patients then typically return several weeks or months later for another laser treatment. During this time the podiatrist will routinely observe the foot and infection. It is also recommended to wear clean socks and shoes and allow the feet to dry and breathe to prevent toenail fungus.
Laser treatment is still a relatively new treatment and not all podiatrists have laser machines. Ask your podiatrist if they do laser treatment for toenail fungus and if it is right for you.
Get Professional Care for a Broken Foot or Ankle
Causes of Hammertoe

Hammertoe, a common foot deformity characterized by an abnormal bending of one or more toes at the middle joint, can develop due to various factors. First, genetics can play a significant role, as individuals with an inherited foot structure that predisposes them to hammertoes may be more susceptible. The choice of footwear is another critical factor, as tight, narrow, or ill-fitting shoes can force the toes into unnatural positions, subjecting the toe joints to excessive pressure. High-heeled shoes, in particular, can push the toes forward into a bent position, contributing to hammertoe development. Additionally, a toe length discrepancy, where one toe is longer than the others, can increase the risk, especially if it consistently rubs against the inside of the shoe. Conditions like arthritis can also lead to joint inflammation and deformities, including hammertoes. Past toe injuries or trauma can disrupt toe joint alignment, and muscle imbalances affecting toe movement can also play a role. If you have developed a hammertoe, it is suggested that you schedule an appointment with a podiatrist for early intervention and treatment to help manage the condition and prevent it from worsening.
Hammertoes can be a painful condition to live with. For more information, contact one of our podiatrists of Podiatry Services . Our doctors will answer any of your foot- and ankle-related questions.
Hammertoe
Hammertoe is a foot deformity that occurs due to an imbalance in the muscles, tendons, or ligaments that normally hold the toe straight. It can be caused by the type of shoes you wear, your foot structure, trauma, and certain disease processes.
Symptoms
- Painful and/or difficult toe movement
- Swelling
- Joint stiffness
- Calluses/Corns
- Physical deformity
Risk Factors
- Age – The risk of hammertoe increases with age
- Sex – Women are more likely to have hammertoe compared to men
- Toe Length – You are more likely to develop hammertoe if your second toe is longer than your big toe
- Certain Diseases – Arthritis and diabetes may make you more likely to develop hammertoe
Treatment
If you have hammertoe, you should change into a more comfortable shoe that provides enough room for your toes. Exercises such as picking up marbles may strengthen and stretch your toe muscles. Nevertheless, it is important to seek assistance from a podiatrist in order to determine the severity of your hammertoe and see which treatment option will work best for you.
If you have any questions, please feel free to contact our office located in Murrieta, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Hammertoe
Hammertoe is a foot deformity that occurs due to an imbalance in the tendons, muscles, or ligaments that are responsible for holding the toes in their normal position. This condition may be caused by poor footwear, foot structure, trauma, and disease. The most common solution for hammertoe is to relieve the pain by changing your footwear and wearing orthotics. In severe cases, surgery may be required.
The shoes that are most likely to cause hammertoe are high heeled shoes or shoes that are too tight in the toe box. Tight shoes will force your toes to crowd together in a curled position. This position will likely continue when you take your shoes off. Another cause is trauma. When you stub your toe, you are increasing the chance that you will develop hammertoe.
There are risk factors that may make you more likely to develop this condition. Women are more likely to have the condition compared to men, and it is also more likely to appear in those who are older in age.
Many different foot problems can be avoided by wearing shoes that have adjustability, adequate toe room, and low heels. Furthermore, if you want to buy new shoes, you should look to purchase them at the end of the day and make sure you know your correct size. The importance of buying shoes at the end of the day is that your feet swell as the day progresses. You should also ensure that you are wearing your correct size because your shoe size may change as you grow older.
To diagnose someone with hammertoe, your podiatrist will need to conduct a thorough examination of your foot. Your doctor may even order an x-ray to evaluate the bones and joints of your feet and toes.
If you have hammertoe, your podiatrist may recommend that you wear shoes that fit you better along with inserts to place inside them. Additionally, he or she may suggest special exercises for you to perform to stretch your toes. One helpful exercise it to pick up marbles with your feet or crumple a towel with your toes.
Prior to meeting with your podiatrist, it will be helpful to make a list of all the symptoms you are experiencing. You should also make a note of medications you are taking and important personal information about your medical history.
Managing a Broken Foot

A broken foot, resulting from various causes such as sports injuries, falls, or accidents, can significantly impact your daily life. With 26 delicate bones in each foot, fractures are common and can lead to changes in physical appearance and movement. Symptoms of a broken foot include sudden or gradual pain, difficulty in bearing weight, swelling, bruising, altered gait pattern, and poor balance. Long-term treatment is needed for effective recovery. It typically involves the use of protective casts, boots, or supportive footwear to shield the foot during the healing process. The healing process for bones usually spans six to eight weeks, though the duration may extend based on the severity of your fracture. Beyond immediate care, rehabilitation exercises play an important role in restoring range of motion, mobility, strength, and balance. Because neglecting proper treatment can result in complications, it is imperative to prioritize comprehensive and sustained care for a broken foot. By adhering to these measures, individuals can optimize the healing process, minimize risks, and regain full functionality, ensuring a smoother road to recovery. If you have broken your foot, it is suggested that you schedule an appointment with a podiatrist as quickly as possible for an exam and appropriate treatment methods,
A broken foot requires immediate medical attention and treatment. If you need your feet checked, contact one of our podiatrists from Podiatry Services . Our doctors can provide the care you need to keep you pain-free and on your feet.
Broken Foot Causes, Symptoms, and Treatment
A broken foot is caused by one of the bones in the foot typically breaking when bended, crushed, or stretched beyond its natural capabilities. Usually the location of the fracture indicates how the break occurred, whether it was through an object, fall, or any other type of injury.
Common Symptoms of Broken Feet:
- Bruising
- Pain
- Redness
- Swelling
- Blue in color
- Numbness
- Cold
- Misshapen
- Cuts
- Deformities
Those that suspect they have a broken foot shoot seek urgent medical attention where a medical professional could diagnose the severity.
Treatment for broken bones varies depending on the cause, severity and location. Some will require the use of splints, casts or crutches while others could even involve surgery to repair the broken bones. Personal care includes the use of ice and keeping the foot stabilized and elevated.
If you have any questions please feel free to contact our office located in Murrieta, CA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.