Causes, Symptoms, and Treatment for a Broken Foot
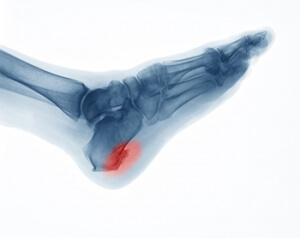
The human foot has 26 different bones, and the foot is divided into three parts: the hindfoot, the midfoot, and the forefoot. Each section of the foot is composed of a different amount of bones. For instance, the forefoot is made up of 19 bones. The midfoot is composed of five smaller bones called the navicular, cuboid, and three cuneiform bones. Lastly, the hindfoot is made up of only the talus and the calcaneus. The feet tend to be vulnerable to slipping and twisting; consequently, fractured bones within the foot are common. When a bone gets crushed, bent, twisted, or stretched it may become broken.
Many foot fractures occur through an accident or trauma. More specifically, common causes for broken feet are car accidents, falls, missteps, or overuse. If you have a broken ankle or foot, you may have one or more of the following symptoms: throbbing pain, swelling, bruising, tenderness, deformities, and difficulty walking.
There are some factors that may put you at a higher risk of developing a broken foot. People who participate in high-impact sports are more likely to develop foot fractures because of the stresses, direct blows, and twisting injuries involved in gameplay. Additionally, those who suddenly increase their activity level are more likely to suffer a stress fracture.
Unfortunately, there are different complications that may arise because of a foot fracture. For instance, arthritis may be caused by fractures that extend into the joints. Bone infections are also possible in open fractures due to the bone being exposed to bacteria. However, there are ways you can help prevent yourself from breaking your foot. One way to avoid fractures is to wear proper footwear. If you plan on going on a run, you should wear running shoes. You should also replace your shoes if you notice that they are becoming worn out. For runners, it is best to replace shoes every 300 to 400 miles.
Treatment for foot fractures usually consists of rest, ice, elevation, and compression (RICE). If you plan on wrapping your foot, try not to wrap it too tightly because doing so may cut off blood supply in the foot. You should also avoid walking on the fractured foot.
If you suspect you have a broken foot, you should see your podiatrist right away. It is important that you have someone bring you to your doctor, since driving with a broken foot can be dangerous. You should especially seek urgent care if you are experiencing numbness, pain, or deformities in your foot.
Gout and Its Causes
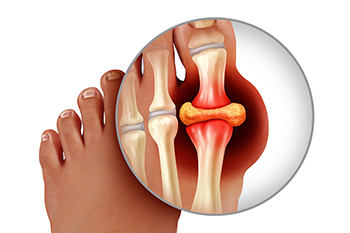
Gout, an inflammatory arthritis, is a condition characterized by sudden, intense pain, redness, and swelling in the joints, most commonly affecting the big toe. The root cause of gout lies in the accumulation of urate crystals in the affected joints, leading to excruciating bouts of pain. Urate crystals form when the body produces excessive uric acid or fails to eliminate it efficiently. High levels of uric acid can result from dietary factors, particularly the consumption of purine-rich foods, like red meat, seafood, and alcohol. A genetic predisposition and certain medical conditions, such as kidney dysfunction, contribute to the likelihood of developing gout. Obesity and dehydration also play roles in exacerbating the condition. Understanding the definition and causes of gout is critical for individuals, enabling them to make informed lifestyle choices and dietary adjustments to manage and prevent the recurrent pain associated with this arthritic condition. If you have developed gout, it is strongly suggested that you are under the care of a podiatrist who can help you manage this condition.
Gout is a foot condition that requires certain treatment and care. If you are seeking treatment, contact one of our podiatrists from Podiatry Services . Our doctors will treat your foot and ankle needs.
What Is Gout?
Gout is a type of arthritis caused by a buildup of uric acid in the bloodstream. It often develops in the foot, especially the big toe area, although it can manifest in other parts of the body as well. Gout can make walking and standing very painful and is especially common in diabetics and the obese.
People typically get gout because of a poor diet. Genetic predisposition is also a factor. The children of parents who have had gout frequently have a chance of developing it themselves.
Gout can easily be identified by redness and inflammation of the big toe and the surrounding areas of the foot. Other symptoms include extreme fatigue, joint pain, and running high fevers. Sometimes corticosteroid drugs can be prescribed to treat gout, but the best way to combat this disease is to get more exercise and eat a better diet.
If you have any questions please feel free to contact our office located in Murrieta, CA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Everything You Need to Know About Gout
Gout, typically found in diabetic patients, is an unusually painful form of arthritis caused by elevated levels of uric acid in the bloodstream. The condition typically strikes the big joint on the big toe. It has also been known to strike the knees, elbows, fingers, ankles and wrists—generally anywhere that has a functioning, moving joint.
The high level of uric acid in a person’s bloodstream creates the condition known as hyperuricema—the main cause of gout. Genetic predisposition occurs in nine out of ten sufferers. The children of parents who suffer gout will have a two in ten chance of developing the condition as well.
This form of arthritis, being particularly painful, is the leftover uric acid crystallizing in the blood stream. The crystallized uric acid then travels to the space between joints where they rub, causing friction when the patient moves. Symptoms include: pain, redness, swelling, and inflammation. Additional side effects may include fatigue and fever, although reports of these effects are very rare. Some patients have reported that pain may intensify when the temperature drops, such as when you sleep.
Most cases of gout are easily diagnosed by a podiatrist’s assessment of the various symptoms. Defined tests can also be performed. A blood test to detect elevated levels of uric acid is often used as well as an x-ray to diagnose visible and chronic gout.
Treatment for gout simply means eliminating symptoms. Non-steroid anti-inflammatory drugs or NSAIDs (Colchicine and other corticosteroid drugs, etc.) will quell the redness, the swelling, and the inflammation. However, managing your diet, lifestyle changes, and using preventative drugs are all helpful toward fully combating the most severe cases.
Those that lead an inactive lifestyle are at a higher risk for gout. Any amount of exercise decreases the probability of repeat encounters with the condition. Reducing your consumption of red meat, sea food, and fructose-sweetened drinks also reduces the likelihood of chronic gout as well.
Ingesting Vitamin C, coffee, and particular dairy products can help with maintaining a healthy lifestyle. There are new drugs out on the market that inhibit the body’s production of uric acid-producing enzymes. However, reducing or eliminating your overall levels of uric acid is the best remedy to ensuring you lead a gout-free life.
Relief for Heel Spurs
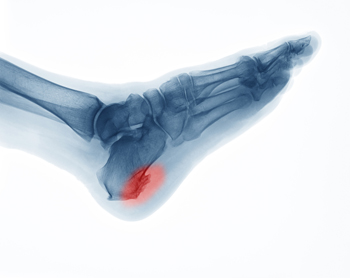
Heel spurs, which are bony growths on the underside of the heel, can cause significant pain and discomfort. They often occur along with plantar fasciitis, a condition characterized by inflammation in the bottom of the foot, particularly in the heel area. To alleviate this discomfort, various treatments and remedies from a podiatrist are available. Cold therapy can help reduce inflammation in the heel tissue. This may be achieved by using a cold compression pack or rolling the foot over a frozen water bottle. Wearing comfortable and well-fitting shoes is essential to reduce pressure on the heel spur. Wearing custom orthotics, prescribed by a podiatrist, can also provide extra heel support. Taking anti-inflammatory medications can help alleviate heel pain and reduce tissue inflammation. Stretching exercises for the calf, surrounding muscles, and the plantar fascia can ease strain and pressure on the heel spur. If you have a heel spur that is causing you persistent pain, it is suggested that you schedule an appointment with a podiatrist for appropriate treatment methods.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact one of our podiatrists from Podiatry Services . Our doctors will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our office located in Murrieta, CA . We offer the latest in diagnostic and treatment technology to meet your needs.
Heel Spurs
Heel spurs are the result of calcium deposits that cause bony protrusions on the underside of the heel. Heel spurs are usually painless, but they have the potential to cause heel pain. Heel spurs tend to be associated with plantar fasciitis, which is a condition that causes inflammation of the band of connective tissue that runs along the bottom of the foot. They most often occur to athletes whose sports involve a lot of running and jumping.
Some risk factors for developing heel spurs include running and jogging on hard surfaces, being obese, wearing poorly fitting shoes, or having walking gait abnormalities.
It is possible to have a heel spur without showing signs of any symptoms. However, if inflammation develops at the point of the spur’s formation, you may have pain while walking or running. In terms of diagnosis, sometimes all a doctor needs to know is that the patient is experiencing a sharp pain localized to the heel to diagnose a heel spur. Other times, an x-ray may be needed to confirm the presence of a heel spur.
Heel spurs can be prevented by wearing well-fitting shoes that have shock-absorbent soles. You should also be sure that you are choosing the right shoe for the activity you want to partake in; for example, do not wear walking shoes when you want to go on a run. Additionally, maintaining a healthy weight can be beneficial toward preventing heel spurs, as it will prevent an excess amount of pressure being placed on the ligaments.
There are a variety of treatment options for people with heel spurs. Some of these include stretching exercises, physical therapy, shoe inserts, or taping and strapping to rest stressed muscles and tendons. If you have heel pain that lasts longer than a month, don’t hesitate to seek help from a podiatrist. Your doctor can help you determine which treatment option is best for you.
Are You Suffering From Nerve Damage?
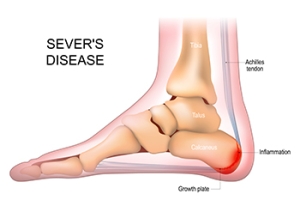
Definition and Affected Population of Sever’s Disease
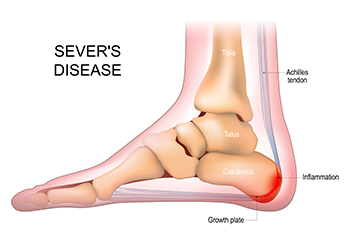
Sever's disease, a common but often misunderstood condition, is not truly a disease, but rather a growth-related heel pain that affects active children and adolescents. This condition, also known as calcaneal apophysitis, occurs when the growth plate at the back of the heel becomes inflamed due to repetitive stress and tension. Children between the ages of 8 and 15 are most susceptible to Sever's disease, as this is typically when their bones are rapidly growing. This growth spurt places extra stress on the heel's growth plate, especially in active children who participate in sports or activities that involve running and jumping. The hallmark symptom of Sever's disease is heel pain, often exacerbated by physical activity. This pain can be particularly bothersome during or after exercise. Understanding Sever's disease is essential for parents and young athletes, as it enables early recognition and appropriate management. If your active child has heel pain, it is suggested that you consult a podiatrist who can effectively diagnose and treat Sever’s disease.
Sever's disease often occurs in children and teens. If your child is experiencing foot or ankle pain, see one of our podiatrists from Podiatry Services . Our doctors can treat your child’s foot and ankle needs.
Sever’s Disease
Sever’s disease is also known as calcaneal apophysitis, which is a medical condition that causes heel pain I none or both feet. The disease is known to affect children between the ages of 8 and 14.
Sever’s disease occurs when part of the child’s heel known as the growth plate (calcaneal epiphysis) is attached to the Achilles tendon. This area can suffer injury when the muscles and tendons of the growing foot do not keep pace with bone growth. Therefore, the constant pain which one experiences at the back of the heel will make the child unable to put any weight on the heel. The child is then forced to walk on their toes.
Symptoms
Acute pain – Pain associated with Sever’s disease is usually felt in the heel when the child engages in physical activity such as walking, jumping and or running.
Highly active – Children who are very active are among the most susceptible in experiencing Sever’s disease, because of the stress and tension placed on their feet.
If you have any questions, please feel free to contact our office located in Murrieta, CA . We offer the newest diagnostic and treatment technologies for all your foot and ankle injuries.
Sever's Disease
Sever’s disease, also known as calcaneal apophysitis is a common bone disorder that occurs during childhood. The disease is defined as an inflammation of the growth plate in the heel. When a child has a growth spurt, his heel bone grows faster than the muscles, tendons, and ligaments in his leg. This disease is a result of overuse. The people who are most likely to be affected by this disease are children who are in a growth spurt, especially boys who are from the ages of 5 to 13 years old. 60% of children with Sever’s disease have both heels involved.
Symptoms of this disease are heel pain that intensifies during running and jumping activities. The pain is typically localized to the posterior part of the heel. Symptoms may be severe, and they can easily interfere with daily activities. Children who play soccer, baseball, and basketball are more likely to develop Sever’s disease.
Your doctor will diagnose your child based on his or her symptoms, x-rays are generally not helpful in diagnosing this disease. Your doctor may examine both heels and ask your child questions about his or her activity level in sports. Your doctor may then use the squeeze test on your child’s heel to see if there is any pain. Nevertheless, some doctors might still use x-rays to rule out any other issues such as fractures, infections, and tumors.
Sever’s disease can be prevented by maintaining good flexibility while your child is growing. Another prevention method is to wear good-quality shoes that have firm support and a shock-absorbent sole. Sever’s disease can be treated by ceasing any activity that causes heel pain. You should apply ice to the injured heel for 20 minutes 3 times a day. Additionally, orthotics should be used for children who have high arches, flat feet, or bowed legs.
If you suspect your child has Sever’s disease, you should make an appointment with your podiatrist to have his or her foot examined. Your doctor may recommend nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen to relieve pain. In more severe cases, your child may need a cast to rest his or her heel. Fortunately, Sever’s disease does not cause long-term foot problems. After treatment, your child should start to feel better within two weeks to two months.
Causes and Symptoms of Foot Blisters

Foot blisters are tiny fluid-filled sacs that form on the skin. They may seem inconspicuous but can be surprisingly uncomfortable, often arising from a combination of factors. Friction stands as a primary cause, especially when ill-fitting footwear or repetitive motion induces rubbing against the skin. Moisture and heat exacerbate the risk, as sweaty or damp conditions soften the skin, making it more prone to friction-related blisters. Additionally, poorly managed moisture, whether from excessive sweating or wet environments, creates an ideal environment for blisters. The symptoms of foot blisters include localized pain, tenderness, and a distinct swelling filled with clear fluid. The affected area may become red, and in more severe cases, the blister may rupture, leading to an open wound susceptible to infection. If you repeatedly develop foot blisters, it is suggested that you confer with a podiatrist who can offer effective relief and prevention methods.
Blisters are prone to making everyday activities extremely uncomfortable. If your feet are hurting, contact one of our podiatrists of Podiatry Services . Our doctors can provide the care you need to keep you pain-free and on your feet.
Foot Blisters
Foot blisters develop as a result of constantly wearing tight or ill-fitting footwear. This happens due to the constant rubbing from the shoe, which can often lead to pain.
What Are Foot Blisters?
A foot blister is a small fluid-filled pocket that forms on the upper-most layer of the skin. Blisters are filled with clear fluid and can lead to blood drainage or pus if the area becomes infected.
How Do Blisters Form?
Blisters on the feet are often the result of constant friction of skin and material, usually by shoe rubbing. Walking in sandals, boots, or shoes that don’t fit properly for long periods of time can result in a blister. Having consistent foot moisture and humidity can easily lead to blister formation.
Prevention & Treatment
It is important to properly care for the affected area in order to prevent infection and ease the pain. Do not lance the blister and use a Band-Aid to provide pain relief. Also, be sure to keep your feet dry and wear proper fitting shoes. If you see blood or pus in a blister, seek assistance from a podiatrist.
If you have any questions, please feel free to contact our office located in Murrieta, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Blisters
Blisters are small pockets of fluid that occur on the top layers of the skin for several reasons. Friction, burns, and diseases are all known causes of blisters. Smaller blisters are known as vesicles, while larger blisters are referred to as bulla. The fluid inside the bubble can be blood, pus, or serum; which is a clear liquid that protects the skin. In most cases, blisters are not a major health issue, but they can be an indicator of a more serious condition.
Causes of blisters vary. Blisters are commonly caused by wearing poorly fitted shoes that rub against the foot. However, there are many other causes besides from friction; including burns, sunburn, insect bites, frostbite, poison ivy/oak, chemical exposure, impetigo, eczema, viral infections, and more.
Most blisters heal by themselves and do not require immediate medical care. If you have a blister, do not pop it since this may cause infection; it is advised to put a bandage over the blister to protect it. If the blister is large, causes pain, or if you have a fever, it is recommended that you see a doctor who can provide proper care. Blisters are easy to diagnose, and if considered prudent by the doctor, can easily be drained of fluid with a sterile needle as well.
To prevent blisters on the feet, wear shoes that fit properly and don’t cause rubbing. Socks can help prevent friction and it is recommended that you wear them if you are wearing shoes. Hand blisters can be avoided by wearing gloves during activities that cause friction against the hand. If you have a blister that pops, do not remove the dead skin, wash the area, apply antibiotic ointment, and cover with a bandage. It is okay in most cases to not seek immediate medical care for a blister if it was just caused by friction. However, if the blister causes pain or does not go away, it is suggested that you see a doctor for a diagnosis.